William O’Connor: We’ve got a really special episode on the podcast today for everyone. As this is our first time, we have two guests on the podcast: Dr. Mo Shaik and Dr. Brittney Newby. They are both Chief Residents of Pediatrics at the Children’s Hospital of Philadelphia. Great to see you both and welcome to the podcast.
Mo Shaik: Thanks Will. Thanks for having us.
Brittney Newby: Yeah, it’s a pleasure to be here, Will. Thanks so much.
William O’Connor: Yeah, thanks. Brittney, I’d love to start with you. Tell me a little bit about your background and how you got into medicine and then how you got into pediatrics.
Brittney Newby: Sure. So, as Will said, I’m Brittney. I’m originally from Atlanta, Georgia but have always had an interest in medicine, particularly pediatrics. I actually ended up doing an MD PhD because I’m very interested in research and moving medicine forward. So I was able to do my MD PhD at the University of Florida, focusing on immunology.
William O’Connor: How long did that MD PhD take? I have a ton of respect for MD PhDs. I just remember as a medical student going and seeing some of these people taking 7, 8, 9 years. How long did it take you, Brittney?
Brittney Newby: It took me eight years. Yeah. All of my twenties. But it was a wonderful time. And it is still some of my fondest memories and was really a solidification of my interest in pediatrics and research. And I’m happy to be continuing that trajectory here at CHOP, where Mo and I have spent the last four years together here as residents and now as chief residents. But moving forward, I’m very interested in autoimmune disease and how that develops, and I’ll be spending my time doing pediatric rheumatology moving forward. So, I’m super excited about it.
William O’Connor: Amazing! Thanks for joining us, Brittney. Mo tell us a little bit about yourself
Mo Shaik: Oh my God, that’s a tough act to follow.
William O’Connor: I know it sounds like it but you got the PhD as well.
Brittney Newby: He’s just as impressive. Don’t let him tell you otherwise.
Mo Shaik: I don’t know about that. No, I also happen to have a PhD and so my interests in pediatrics are probably a little bit newer than Brittney’s. I was a biomedical engineer in college and my PC was also in biomedical engineering and I really wanted to figure out how I could bridge the two worlds of engineering and medicine. Pediatrics seemed like the best place to do it. Both for the things that give me joy and bring me sort of fulfillment – taking care of kids and getting them better – there’s really nothing quite like it. And also, moving the field forward. From my perspective, from an engineering principal sense, device development and things of that nature. So it’s been quite the journey. I’m really happy to be here. This July I’m starting a critical care fellowship, pediatric critical care fellowship at the University of Pittsburgh. So I’m looking forward to continuing the journey.
William O’Connor: Nice. Wow, that’s both amazing backgrounds. I’m just a simple bone doctor here, so I’m definitely the dummy in the shoot today. Tell me your experience so far about being a chief resident.
Mo Shaik: I’ll go first. Brittney, you can fill in the holes that I’m going to have. It’s been quite the journey. It is a year of really leadership training that is compressed. It allows us to experience the breadth and depth of stakeholders across the institution, across our institution, which happens to be a big institution in terms of people’s values, in terms of people’s sort of what they want out of their own lives, what they want out of their work and holding that all together and learning how to work within that system to get our residents trained and have them enjoy the experience too. It’s really quite the learning experience, but I will say it’s been transformative.
Brittney Newby: Absolutely. Yeah, I have to agree with Mo. It truly is a crash course in leadership development, one with a very steep learning curve. It’s been really nice to serve in a role, particularly to advocate for our residents to truly hold their interest and also take those interests and try to advocate on an institutional level. The majority of our group has really found joy in that aspect of chief resident year. Of course, the year also comes with lots of administrative tasks which we’ve all gotten very efficient at completing, so all around, a very transformative year.
William O’Connor: Yeah, that sounds, no, it sounds like you’ve both had a great experience doing that. And I just, it’s one of the things that’s hard because you’ve been studying science and medicine your whole lives, and all of a sudden you’re thrust into this leadership position and have a lot of responsibilities. And I think people underestimate sometimes a lot of the extra burden and administrative burden that you both carry. Talk to me a little bit about some of that burden, in particular as it relates to scheduling and how you keep everyone organized to make sure that you have coverage, people are doing the rotations they need. How have you been dealing with that?
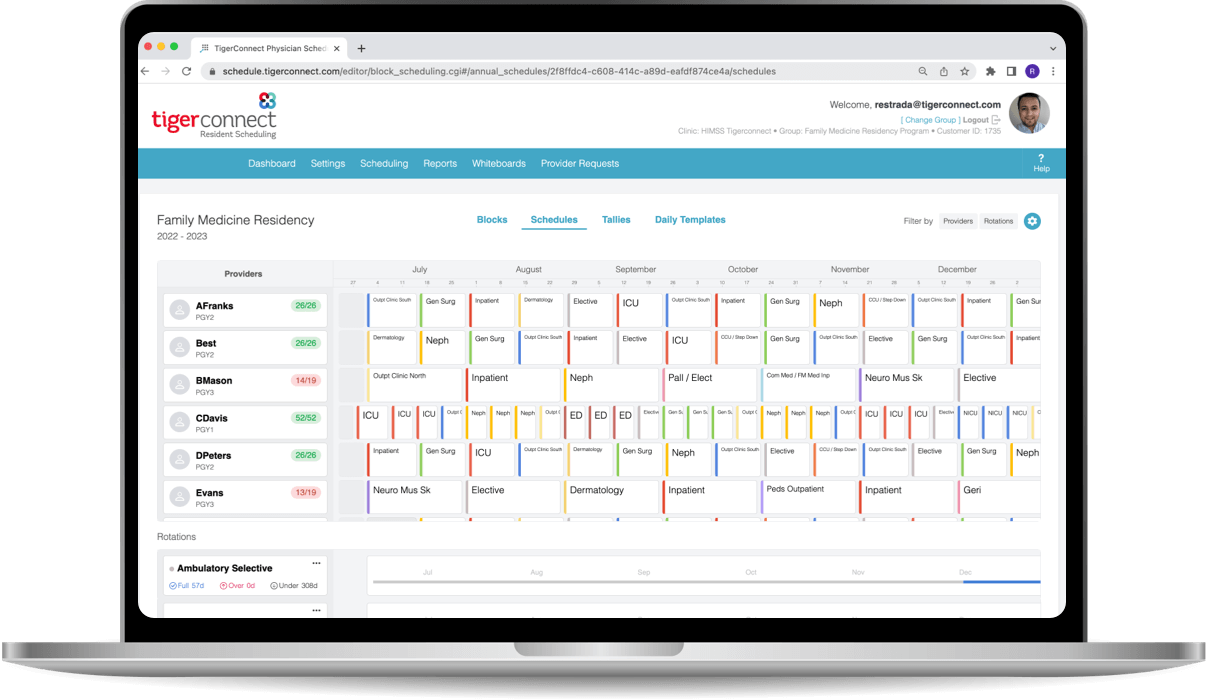
Brittney Newby: Yeah. So when we came into the role, we realized that it was a Herculean task. And Mo, being our engineering mind and our numbers and data guy, was like “hey, I think we can leverage some automation to improve our scheduling workflow”. And he can probably speak a little bit more about the nuts and bolts of that. But I think, in particular, what makes scheduling challenging is one, you have the educational requirements that all residents have to meet, right? It’s foundationally like learning all of your ACGME requirements and making sure that everyone hits every rotation and every requirement that they need. But then you also have to balance people’s lives, right? Residency continues on, but life does not stop while you’re in residency. And I think the hard part is really trying to balance what people need professionally and personally, while also making sure that they meet their educational requirements. And Mo, feel free to jump in.
Mo Shaik: Yeah, no. I think that Brittney hit the nail on the head. That is one of the hardest things to balance. We have to get the residents trained. That’s the requirement, right? That’s 90% of our job. But at the same time, they’re humans too. People need to get married, have kids, and people want to be able to spend time with their loved ones. Sometimes there are major life events that happen, like Britney alluded to, and we have to accommodate for that. We consider that just as much a major part of our job as making sure they get their training. That’s really hard, not to mention that staffing the hospital is also part of our responsibility. We need to make sure the patients on our floors are covered by the providers, which oftentimes are residents, in a way that is safe, effective, and efficient. This requires us to talk to a lot of people across the hospital to make that happen. So yeah, it is herculean.
William O’Connor: Scheduling and getting everyone’s schedule, sounds like a menial task, but to listen to both of you describe it, it has staffing implications throughout the hospital, which translates to quality of care and training implications for all the residents to make sure everyone gets the appropriate amount of training. And that can be pretty complex to make sure everyone’s getting the right number of hours and rotations. Then, as you said, you’re dealing with a bunch of humans and life goes on. Really sounds like a big challenge getting that right. And then personally for you, it’s a lot of hours to create those schedules. Talk to me about that a little bit.
Mo Shaik: Yeah, it is. Brittney’s laughing because it was quite the three months. But effectively, for us, we start the chief year a few months early into our third year of residency. And I will say, we spent a majority of those months working on schedules. What I’m talking about is 90-plus hours a week, Saturdays, Sundays, having a lot of conversations with a lot of different people. It’s exhausting by the end of it, but it’s fulfilling. It really takes a lot of time to do and to do well, and it definitely took us a long time.
William O’Connor: Yeah, when you mentioned 90 hours a week, it gave me a little shiver of memory of those days. Talk to me about your individual wellness and your journey there. Cause you both have had a long time going at this, right? Brittany, did you hear me say it right? You basically gave up your twenties to do this. Talk to me about how you think about that for you personally and also how you are translating that into the program at CHOP.
Brittney Newby: Yeah, that’s a great question. And I think it’s something that has evolved over the years. I think, really we talk about this throughout residency, but really taking hold of your values and I think that that’s one thing we did really well as a group- as a chief group at the beginning. We sat down, talked about our individual values, what was most important to us, individually and as a group, and how we wanted to carry out our vision and values for the year. Our biggest thing we wanted to convey this year was authenticity: being as authentically ourselves in our roles while also building community and fostering a program where everyone’s looking out for each other. And I think that has worked out really well. It also speaks to our individual personalities. The other thing I will say is that residency you work a lot of hours. What I did not expect this year as a chief is the amount of tasks we have. Naturally, your job bleeds into other aspects of your life. So, I think even more this year we’ve had to work hard and make sure that we keep those values and keep those boundaries. And I think that’s something we try to teach and convey to the residents as well.
Mo Shaik: Yeah, boundaries are hard. We’ve had to work very hard to say, “okay, look, I might be working this Friday night, but tomorrow I’m off. And I’ll turn it back on again on Monday and go”. It’s been a journey, but I think we’ve gotten better at it. Brittney, would you say?
Brittney Newby: I think so. Yeah, yeah, I definitely think so.
William O’Connor: You have definitely a bunch of lucky residents underneath you. This is not, I don’t think, the norm to have people worried and concerned about authenticity and that sense of community. So, good on both of you for creating that type of environment at what can be a super stressful time of your life, working all those hours and having to deal with everything else that people have going on. Personally, I think it’s a huge credit to both of you that that is the type of environment you’re fostering. I want to shift gears a little bit and get each of your takes on AI in medicine. It seems these days every two weeks it’s something new. In just six months, we went from ChatGPT 3.5 that barely squeaked by the USMLE exam, to impressing so and then six months later acing it with ChatGPT 4. The level of AI advancement here is extraordinary and not something I’ve ever seen in any other technology. Talk to me a little bit about your thoughts there and what it can do for you administratively, but also as you’re practicing medicine. Where do you see this going?
Mo Shaik: Brittney and I have been using ChatGPT a lot lately. We love using it. I think it’s a hard question to answer. It’s a relatively new technology with a lot of demonstrable use cases across all industries in transformative ways. I think the question and the challenge really is, in healthcare, new technologies are adopted generally a little bit more slowly and deliberately, partially because there are questions about reliability, reproducibility and accuracy. And I think those challenges are important to address. However, I personally am very excited about the future. There’s a paper I was reading recently called ‘ChatGPT but for querying or asking EHR questions’, where the idea is you ask, for example, “What was this patient’s trend of this lab value for the past few days?” It queries the database, the EHR, either structured or unstructured, and walks you through its thought process and spits out that answer. As a future ICU fellow, being able to quickly get large pieces of information quickly is quite exciting to me. Brittney, what do you think?
Brittney Newby: Yeah, I’m particularly excited about it. I certainly agree that in medicine, we’re typically slow adopters, right? Because we have human lives at stake and we’re taking care of people. However, in the administrative role, I think I could also see a very cool application for using AI technology, which is already being used in research spaces. I love the idea of using ChatGPT or other AI interfaces for administrative tasks. You could literally type in a query to ChatGPT and ask it to write a script or code that would potentially take hours and hours to write. So I think that it could certainly improve our efficiency. And I’m excited to see where the automation field goes over the next couple of years. I definitely think we’re always gonna need a human brain operator behind it, especially if you’re using it in medicine or in another field where there’s so much impact. So, to be determined.
William O’Connor: Yeah, Brittney in your area, I was thinking immunology, a lot of autoimmune diseases, right? Have you seen any hope in helping with differential diagnosis?
Brittney Newby: That’s a great question. I think if we, one of the things that the rheumatology division has been working on in many of the divisions here at CHOP is trying to understand data and use it in a way that we can create a reliable disease score or activity score. And I can foresee using something like automation to integrate data from the EMR to plug into a validated disease score activity to give us a little bit of information about, perhaps, JIA severity or whether someone is developing an inflammatory state or a macrophage activation syndrome. So I could certainly see a lot of different applications there. And there are some, not as sophisticated as chatGPT, but there are some programs out there that do attempt to, based on symptomatology, try to give you a list of differentials. So, I can see that it could be more robust with a technology like this.
William O’Connor: No, I think it does. You’re right. I think you’re both right. It just, it really remains to be seen where you know where it’s gonna go next. I know you’ve been in your chief year now for over a year. Sounds like it’s been an incredible experience. Tell me a story or two, each of you from that year that really sticks out in your mind.
Brittney Newby: You want me to take this one first, Mo?
Mo Shaik: Yeah, go ahead Britt.
Brittney Newby: Yeah. Throughout the year, as we alluded to, chief year is a crash course in leadership development and also the quintessential middle manager role. And so sometimes it does feel like you’re put in precarious situations when you’re relaying information to the residents or relaying things to the administration. One of the things that really sticks out in my mind is that, recently, we’ve been onboarding our Rising Chiefs and we were informing the current residents of the transition that is happening. And one of the residents turned to me in a panicked voice and said, “Wait, you guys are done. You guys aren’t leading us yet, are you?” I paused and said, “No, we have a couple of months left and we’ll still be here, we’ll still be the Chiefs until June.” They had this huge sigh of relief. And for me, that was the pinnacle moment of the year because at times it really does feel like you don’t know whether or not you’re making the right decisions or doing the right thing or if residents are really happy with us. And so it was really nice because they turned to me after that and said, “We’re really gonna miss you guys. You guys are an amazing chief class. You’ve really made our intern year a good one.” At that point, I felt like we’d accomplished our goal and it made me smile. It was a nice validating moment.
William O’Connor: Nice.
Mo Shaik: Yeah, I have to agree with Britt. It’s one of those years where you don’t really get feedback on how you’re doing, right? Through residency, there’s always some kind of evaluation and frequent feedback, but no one really tells you how you’re doing in your first year, right? Because there really is no mechanism for that. And so it’s really hard to know how we’re doing, whether we’re actually doing what we set out to do early on. And I agree with Britt. I had a couple of similar interactions where people either texted or emailed me and went, “Hey, so are you guys done? I have questions about my life and my schedule and I can’t, like, when are you starting your fellowship? I really need to meet with you before that.” And I was like, “I didn’t even know you liked me.” So it’s been really nice to know that, at least in a small way, we’ve impacted people’s lives, our residents’ lives, and hopefully made them a little bit more manageable during a very intense training program. And as long as we’ve actually accomplished that, I’ll sleep happily at night.
William O’Connor: Mo, Brittney, thank you so much. You both have been so generous with your time, and I know how precious time is during your residency and chief year. Thank you for joining us today. I enjoyed our conversation.
Brittney Newby: Yeah, thanks so much for having us, Will. This was a blast!
Mo Shaik: Thank you, Will.