Will O’Connor: But in TigerConnect, because we know where everyone is, we know what everyone’s job is, we have their schedule, we have their persona, we’re getting the right information to the right person at the right time.
Mary Ann Borer: Hi, I’m Mary Ann Borer with HIMSS. Today I’m joined by Dr. Michael Davis, Associate Chief Medical Information Officer for Acute Care at Tufts Medical Center, and Dr. Will O ‘Connor, Chief Medical Information Officer at TigerConnect. And we’ll be talking about operating room efficiency, how Tufts Medical Center improved OR workflows.
MB: Before we start, I want to say thank you to TigerConnect for sponsoring this podcast. Tufts Medical Center, part of Tufts Medicine, is an internationally respected academic medical center that has provided patient-centered care in New England for over 200 years. With more than 100 specialties including a top -heart transplant center and a level one trauma center.
MB: Tiger Connect transforms healthcare with the industry’s most widely adopted clinical collaboration platform uniquely modernizing how doctors, nurses, care teams, patients, and data connect with a comprehensive range of solutions including care communication and patient inclusion. scheduling, alarm notifications, nurse call and more, Tiger Connect enhances efficiency, lowers expenses, and ensures safe, reliable communication. Dr. Davis, Dr. O ‘Connor, thank you both for joining us today.
Michael Davis: Thank you so much for having me.
WO: Thanks for having us.
MB: Thank you. Dr. Davis, could you please tell us a little bit about your role and about Tufts Medical Center?
MD: Absolutely. Absolutely. So I’ve been at Tufts Medical Center now, which is in the heart of Boston, Massachusetts, since 2016 when I started my internal medicine residency here. And then I stayed on for an additional year to do a chief residency year as part of the internal medicine residency program. And then after that, I stayed on as faculty. Since then, I have been a part of the Division of Hospital Medicine at Tufts Medical Center as an adult medicine hospitalist, which is sort of 25 % of my total time. And then the other 75 % is split between my role in clinical informatics as the Associate Chief Medical Information Officer for Acute Care, which involves both inpatient emergency services and in perioperative services, and then my final role is as the director for inpatient systems for the department of medicine at Tufts Medical Center.
MD: So I love it here. That’s part of the reason why I haven’t left yet and why they haven’t kicked me out, thankfully. I think being at a place like Tufts Medical Center in the heart of Boston is pretty amazing to see the impact that we have on the community and then the people that we serve around here, it feels kind of like a close knit community type of hospital. but it’s an academic tertiary care center, a level one trauma center doing really amazing things with heart transplant, kidney transplant, and now liver transplant, mechanical devices. We’ve got a really extensive ICU program here, but also as part of my role within Tufts Medicine, I’ve gotten to know the community hospitals at Lowell General Hospital and Melrose Wakefield Hospital through my clinical informatics role. So it’s been a really great seven plus years since being at Tufts Medicine.
MB: Terrific. Can you tell us a little bit about what type of patients you treat and how the medical center supports the community?
MD: Yeah, they’re really sick for sure. So I’ve sort of alluded to it. We’ve got a really impressive cardiac transplant program here and I know as an intern and a resident rotating through the cardiac care unit, here at Tufts Medical Center, how sick these patients are, and how, you know, some of the life -saving measures that we’re doing for these patients, how incredible it is, and how, you know, we’re really living at the cutting edge of technology and being able to keep these patients alive with mechanical devices and mechanical support. And it really feels I’ve sort of alluded to this, like they’re, you know, the people that live around here like their community hospital So you know in addition to all these amazing things that we’re doing on the inpatient side and in the ICUs We’ve got a really great Wide footprint across the community as far as our primary care services go And that extends all throughout Tufts Medicine and all the community Practices that we have across Massachusetts.
MB: That’s wonderful. So I’m sure that with that kind of patient and all the specialists that are involved, I’m sure that you have some communication challenges. Can you describe some of the communication challenges that clinical teams can face in that hospital setting? And what does care coordination look like?
MD: Yeah, it’s a great question. So I could sort of answer that through the lens of just that Tufts Medical Center or any of the individual hospitals. But I could also answer it through the lens of Tufts Medicine as a sort of a network of providers across Massachusetts. So approaching it at the hospital level, because that’s what I know best as a medicine hospitalist, I really like how Tiger Connect is considered to be a clinical communication and collaboration platform because that’s really describing what it does.
Like I think we face so many challenges when it comes to frictionless communication and team between care team members in the hospital. And with legacy technologies like pagers, which are sort of unidirectional, where you send a page to somebody, and then you are sort of tethered to your landline waiting for them to maybe hopefully magically call you back to get an answer about a really sick patient.
MD: When you’re trying to work as a team, that introduces a lot of efficiencies. and so with a solution like Tiger Connect where you are able to securely send messages between care team members on your phone on the fly at the bedside if you need to stay at the bedside with a really sick patient to me that’s what supporting this frictionless type of collaboration and communication between care team members is all about.
MB: Terrific now, how are you using Tiger Connect? to solve some of those communication challenges during say operating room workflows?
MD: In my role as associate CMIO for acute care, I’ve really forced myself to try to understand at least the challenges that perioperative staff and surgeons, anesthesiologists, or nurses, techs in the OR have faced for so long. Because to me, I was sort of ignorant to all of those challenges through my training as a medicine physician. And it’s clear to me that there are so many moving parts and, you know, as all hospitals try to manage many different ORs on any given day, the importance of synchronous communication and collaboration has never been more important to make sure that we’re able to operate on these patients smoothly and move from, you know, one case to another. to the next in a timely and safe manner.
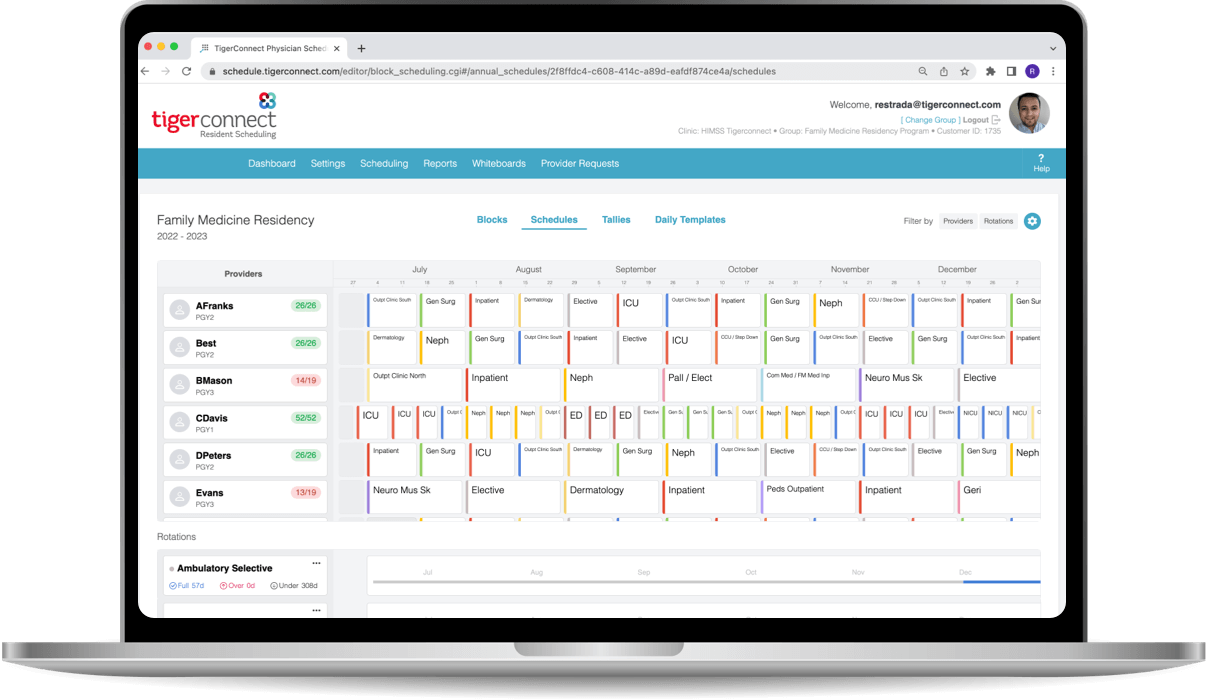
MD: And it was about a year ago, I think, when we started to talk with some of the leaders in the periop services here at Tufts Medical Center about the challenges that they were facing, specifically with OR throughput. And when we really drilled into it, it turns out that any one patient’s life cycle through the OR involved 17 different individual phone calls being made. And to me, you know, that is with 17 different phone calls, you’re sort of introducing a lot of inefficiencies and a lot of waste into that single patient’s life cycle through the OR. And we started thinking more about how we could, you know, make the OR staff’s life easier. and more automated. And so that’s when we started to come up with a solution of sending automated notifications to all of the staff’s Tiger devices or Tiger accounts on their personal or shared phone devices, alerting them when certain things were being done in the OR that would indicate that it was time for them to arrive to the OR to perform their specific job.
WO: Yeah, Dr. Davis, I think that’s a really good point, and that’s where we focused with you to make sure that we were making that a seamless process. So through the integration with your EMR, when the patient’s being registered, when they’re done with pre -op, it could be the patient check -in, the OR set up, the arrival, the closing, the leaving. All of that sends off automated messages from your Epic EMR to TigerConnect, but in TigerConnect, because we know where everyone is, we know what everyone’s job is, we have their schedule, we have their persona, we’re getting the right information to the right person at the right time, relative to those seven steps. So instead of having to make 19 or 20 or 25 phone calls, all of that communication inefficiency is gone. And that ends up speeding that process. And you move the patients through the OR process that much faster.
MD: Yeah, that’s exactly right. And I think one thing to really stress here is that we eliminated those 17 different phone calls in lieu of the eight total automated notifications being sent to Tiger. We did not add any work. So those Tiger notifications are being generated by case tracking events that the OR staff is already doing in the EMR to begin with. So it’s to me like that’s the beauty of these event -driven notifications from the EMR to Epic. No added work is being done. This is work that’s already happening and we’re just capturing that work through the documentation into discrete fields by the OR staff and generating tiger notifications to the appropriate people at the appropriate times.
WO: And I think that’s a really key point in why you’ve gotten such good adoption because unlike the EMR that requires people to do a lot of work, this didn’t require anyone to do any extra work. The notifications being driven from the EMR are automatic and I think that’s really what clinicians are working on. for is a way for this technology to speed them up instead of slowing them down.
MD: Exactly.
MB: That’s remarkable. You can really see how that would drive a lot of inefficiencies. Dr. Davis, can you share any tangible results or metrics that showcase the improvements in these OR workflows and other workflows since implementing TigerConnect?
MD: Yeah. So, to start with the operating room efficiency metrics, like big shout out to our perioperative services team and specifically the director for the periop services. He’s been hugely helpful in tracking these metrics just to see how we’re doing and keep us honest, as we always want to improve upon the things that we’re doing. And so specifically we’ve looked at the turnover time of all cases and also the first case on time starts right for the OR at Tufts Medical Center. And we had seen that, you know, so we introduced this Tiger workflow back in March of 2023, both the turnover time in the first case on time starts sort of stayed flat for the first couple months. And then to the credit of the PERIOP services leadership team, they had also introduced a pilot of staggered OR start times in July of 2023. And then once that hit, we saw a significant improvement in the first case -on -time starts rate. I think it was roughly a 70 % increase in the rate of first case -on -time starts.
MD: So huge shout -out again to the PERIOP staff here at Tufts Medical Center.
MB: Fantastic. And Dr. Davis, can you also describe how Tire Connect has impacted communications within other departments at Tufts? And maybe you can share a specific improvement metrics if you’ve got them.
MD: Yeah, absolutely. So one thing that comes to mind is our radiology alerts. So anytime a patient across the system at Tufts Medicine, so Tufts Medical Center, Lowell General Hospital or Melrose Wakefield Hospital, undergoes a radiology test, there’s the possibility that something is found on that radiology test that requires additional follow -up by the provider to order that test. And that additional follow-up sort of ranges across the spectrum of acuity and how quickly that provider needs to follow something up.
There’s yellow alerts, which are sort of incidental findings that should be followed up, or at least acknowledged by the ordering provider when within 36 hours. A lot of times these are dealt with after discharge, sort of low acuity types of things.
MD: And then you have orange alerts which should definitely be followed up within 12 hours and before the patient is discharged but might not necessarily be a matter of life and death where you need to follow up within an hour. That is a red alert. So red alerts are things like, you can imagine doing a CAT scan of the head because somebody’s a little bit confused and then incidentally, or maybe not even incidentally, but surprisingly you see a bleed in the head that requires the order and providers immediate attention because they might have to intervene upon that bleed very quickly. That is a red alert that will be generated.
MD: So historically at Tufts Medicine, these alerts, you know, red, orange, and yellow, were sent to providers’ emails or pagers. And we had noticed in working with our radiology team that there was pretty poor compliance or at least, you know, compliance rates that we really felt could be improved upon in acknowledging those different alerts within the targeted acknowledgement window. So we want people to acknowledge yellow alerts in 36 hours, orange alerts in 12 hours, and red alerts in one hour. For orange alerts specifically, we had found that only 65 % of the alerts were being closed out, meaning acknowledged by the ordering provider within the compliance window. We then worked really hard with the technology staff and with another third party vendor called Nuance, which sort of helps generate these alerts in replacing pager for the provider’s primary device of being notified that there is an alert with TigerConnect.
MD: So anybody who had pager listed as the way that they should be contacted about a radiology alert suddenly had Tiger as the way that they were gonna be contacted. And this occurred about one year ago. What we had noticed, and specifically for those orange alerts and switching from pager to tiger, we saw a pretty impressive improvement in closing out those orange alerts within the compliance window. So it went from 65% with pager to 87% with TigerConnect. And that improvement has persisted over the last few quarters. So it looks, you know, knock on wood to be a pretty sustainable improvement.
MB: Yeah, it really is an improvement. Dr. O ‘Connor, could you maybe tell us a little bit about how TigerConnect is helping healthcare organizations automate clinical workflows and remove some of the barriers to healthcare communication?
WO: Sure. That’s a good question. Our focus is really on a solution and engineering value. The technology for us is easy at this point. So we’re not focusing on the product and technology, but rather getting verified outcomes for our customers. And you really heard Dr. Davis talk about it, 70% improvement in first case how time starts. That’s what we’re after. And clinicians don’t want more technology like an EMR. That’s already a big enough burden for them, and they’re spending so much time in the EMR. As you heard us talk about earlier, they want something that’s automated for them, that provides value, that provides time savings, that provides things that improve the cost and the quality and experience of care. So we build and deploy our technology to do just that. Dr. Davis used the perfect word, frictionless. We want it to be frictionless and that’s what we provide. So we automate these workflows in a way that doesn’t require extra work by the clinicians. We remove barriers to make communications fast and seamless.
We make it easy to find people, to connect and collaborate with them. And we make it easy to get the right information to the right person at the right time through this automation.
MB: Excellent, then we heard a little bit about this from Dr. Davis earlier, but could you maybe tell us a little more about the importance of operating room workflows and what could be at stake from poor or incomplete communication?
WO: Yeah, they’re critically important to every hospital. There is a huge financial impact of surgical delays and delays in the operating room. Roughly, 70% or so of a hospital revenue comes from the OR. So if you have delays, that means that the OR can’t do as many cases, and that has a direct impact on the financial health of a hospital. So things like first case on time starts are important, we’re after with this technology improving room turnover time. We’re improving PACU bed holds. We are improving getting people out of the PACU up to the floor. We’re improving the amount of staff overtime that you need because we’re doing things faster and ultimately we’re able to provide the ability to our customers for them to do more OR cases. More add-on cases, more emergency cases, which is going to improve the health of their patients as well.
MB: Absolutely. Dr. O ‘Connor, how do you see the future of healthcare communication evolving, particularly as we see greater adoption of automation and automated solutions?
WO: You know, I think what you’re seeing here is really exactly what Dr. Davis was describing by replacing 17 phone calls that take a lot of work and it’s a lot of toil for people sitting there and waiting. They’re replacing those with seven automated steps that require no work by the end user at all. And when you do that for clinicians, they notice. So what I think we’re going to see is you’re going to see continued adoption of these purpose -built systems that sit separately. They sit outside of an EMR. We know at this point that communication and collaboration is a primary use case. It’s important enough and valuable enough to have these systems sit and be adopted on their own and having communication and scheduling and persona all on the same platform, I really think because these systems are so valuable, you’re gonna continue to see an uptick in their usage and adoption.
MB: Excellent, Dr. Davis, Dr. O ‘Connor. Thank you both for joining us today and thank you for sharing your insights with us.
WO: Thank you very much.
MD: Thank you so much for having us.
MB: And of course, special thanks to Tiger Connect for sponsoring this podcast. Have a fantastic day rest of your day.