For all the progress we’ve made digitizing healthcare—connecting systems, virtualizing workflows, and modernizing the clinical tech stack—one stubborn truth keeps resurfacing: communication in healthcare is still far more chaotic than it should be. Even with sophisticated tools in place, clinicians continue to wrestle with gaps, delays, and misdirected information that compromise care and drain precious time and attention.
This isn’t a problem of intent. It’s a problem of design.
And importantly, it’s a problem that technology alone hasn’t solved.
In the first article of this series, I explored why nurses should not be middleware—a situation that persists when fragmented systems force clinicians to manually bridge gaps between alerts, devices, and teams. In this second article of our series on Healthcare Communication Orchestration, I want to examine why disordered communication remains so pervasive, why the stakes are rising, and why the path forward requires more than adding new channels or devices—it requires rethinking the entire coordination layer that underpins clinical work.
Why This Still Matters
Despite the widespread adoption of EHRs, secure messaging, and clinical decision support tools, communication breakdowns remain one of the leading—and most stubborn—drivers of safety events and operational inefficiency.
Here’s why the problem persists:
1. Patient safety risks continue to surface.
Communication failures remain a top contributor to preventable harm, even in highly digitized environments. ¹ ² Clinicians still struggle to deliver the right information to the right person at the right time—especially under rapid escalation.
2. Malpractice claims haven’t disappeared.
While phone-related errors have declined, clinicians now face a different issue: HIPAA-compliant texting introduces the risk of clinicians drowning in message overload. ³
3. Communication waste slows patient flow.
Inadequate routing, unclear escalation paths, and slow acknowledgment cycles introduce friction across clinical operations. Every delay—whether for a consult, transport, or medication order—creates downstream bottlenecks. ⁴ ⁵
4. Patients experience the fragmentation.
When clinical teams appear uncoordinated or delayed, patients and families feel it. Fragmented communication erodes trust, impacts loyalty, and undermines the perception of care quality. ⁶
5. Humans are not built for multitasking.
Digital notification volume continues to rise. More devices, apps, and popups lead to more distraction—not better care.⁷ Cognitive load becomes a silent safety risk.
6. Alarm fatigue is very real.
“Nuisance” or nonactionable alarms remain a constant source of frustration. Without orchestration, alerts are treated equally—even when their clinical urgency varies dramatically.⁸
These issues are not hypothetical. I’ve seen them repeatedly and personally—at the bedside, in quality and safety governance, and as a CMIO and CHIO working to modernize clinical communication infrastructure.
What I See First-Hand
As a hospitalist, and from working with my Quality & Safety colleagues, I’ve frequently watched my Radiology and Lab Medicine colleagues navigate far too many steps just to identify “who’s on call” to relay a critical result. Those minutes matter—yet they are often lost hunting through EHR schedules.
As a CMIO/CHIO, I’ve piloted many digital solutions aimed at improving communication. Yet, I see my MD, APP, and RN colleagues getting prematurely kyphotic with their faces bent over their “dinging” smart phone as they walk the halls of the hospital, bumping into the WOWs that no one likes to use, asking “please make it stop”.
Simply sending more communication to a mobile device is not ‘smart communication.’
And organizational change is equally difficult. To truly fix this problem, health systems must reexamine:
- Device and mobility strategy
- Policies governing synchronous vs. asynchronous communication
- Training and change readiness
- Platform consolidation to reduce vendor sprawl—not only to reduce TCO, but to be able to support highly-reliable, standard workflows
- Smart infrastructure investments that future-proof new hospital towers
We must double down on the remaining problems of misdirected communication and alarm overload.
A Core Solution: Orchestrated Communication
One of the clearest answers is communication orchestration—a precision-driven approach to routing only the right information, at the right time, to the right role, based on context.
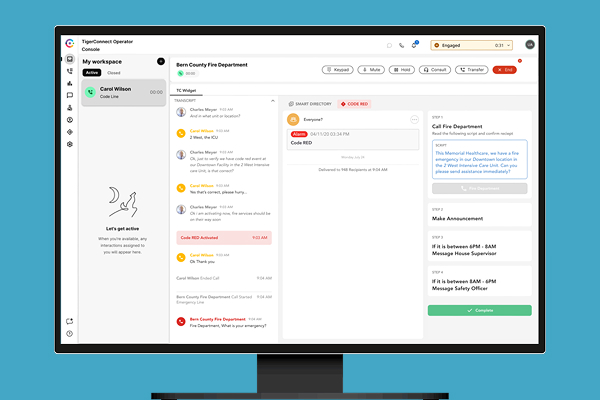
This is not a future ideal. It’s available today. TigerConnect’s platform supports this through:
- Intelligent routing to reduce response times
- Reduced noise by supressing lowvalue alerts
- Persona management (roles, teams, schedules, escalation logic) to prevent misdirected communication
When orchestration is applied, the results are significant:
- Less distraction and cognitive switching
- More time for patient-centered care
- Greater team coordination across the care continuum
A Realistic Scenario — Orchestration in Action
To illustrate the power of orchestrated communication, consider this scenario:
Sandy Jones (Patient 1) is a patient with a high-risk airway, now POD#1 from a radical neck surgery and a complicated tracheostomy placement. It’s Saturday night. Sandy is on a ventilator. The early warning alarms were just triggered by both the ventilator monitor and the capnography monitor. The “Alarm Orchestration Engine” detects these two alarms combined as a “high-likelihood risk”, and per protocol, automatically texts the assigned primary RN and Respiratory Tech to evaluate the patient.
Bob (Primary RN) receives a “High Risk Airway Alarm” text on his mobile device, Bob presses “acknowledge” and selects “headed to bedside” quick response to indicate he is in route.
Respiratory Tech is on the same thread that Bob is on; he presses “acknowledge” and selects “headed to bedside” quick response to indicate that he is also in route.
Both the primary RN and Respiratory Tech have just responded within the 1-minute escalation period that they are on the way to the bedside. Thus, the High-Risk Airway Protocol is activated for Sandy. The Alarm Orchestration Engine is now waiting for the next event in the protocol for Sandy, whether to text the covering Head & Neck surgeon on call.
Bob (Primary RN) is also covering three other patients (Patients 2-4), and they are about to have some low to moderate risk issues that will also potentially trigger simultaneous alarms….
As Bob (Primary RN) is rushing to Sandy’s bedside, Patient 2 triggers the Falls Detection System. The “Alarm Orchestration Engine” knows that Bob is on the move to Sandy’s room for a high-risk event and recognizes that Patient 2’s alarm is of Medium risk; therefore, it proactively anticipates the need to alert Jenny (RN) to cover for Bob.
Bob (Primary RN) receives the text notifying him of a “Medium Risk Fall Alarm” for Patient 2. Recognizing he needs backup, he could text Jenny directly, but instead selects “Call Nurse Jenny for Back-up” and does a quick VOIP call to give additional context. “Hey, Jenny, thanks. I’m headed to Room 235, high-risk airway. Heads up, <Patient 2> fell yesterday and is on aspirin. Will follow up with you.”
Jenny (RN): “Got it. Headed there now.”
Held alert: Meanwhile, Patient 3 has post-op pain and is on a PCA pump. He has pushed the button for a dose, but his pain is still a 4 out of 10. He pushes the Nurse Call button on his bedside tablet. The Alarm Orchestration Engine, seeing that both Bob and Jenny are tied up with higher-acuity events (per protocol), sets a 5-minute timer to release a message to Bob about the patient’s request for pain medication, giving Bob a few minutes to stay focused on assessing the high-acuity alarm. Patient 3 receives a message back indicating the Nurse will be notified shortly and then is updated when the Nurse is notified. In the absence of the concurrent high risk airway alarm for Patient 1, this alert for Patient 3 would have been immediately released to Bob.
Bob (Primary RN) has completed his assessment of Sandy. He added the on-call Head & Neck surgeon to the thread, this was pulled in automatically from the Schedule system, and he sent the following text: See alarm details above. Low ETCO2 of 30. HR 110 and SBP low at 90. Escalating to you. Please advise.”
Avoided alert: Meanwhile, Patient 4 spills her protein shake and requests a clean-up of her floor. This event is intelligently routed by the Alarm Orchestration Engine directly to Environmental Services (EVS) because that is the assigned role for coverage of this low-acuity event. The patient is messaged that EVS is on the way. Neither Bob nor Jenny are bothered by this nuisance alert.
This scenario demonstrates how orchestration:
- Boosts important signals
- Squelches nuisance alerts
- Dynamically allocates backup resources
- Ensures adherence to clinical protocols
- Reduces cognitive burden
- Improves safety and response time
Additionally, the Alarm Orchestration Engine also provides data for dashboards, enabling system-level insights into response times, bottlenecks, escalation patterns, and protocol compliance.
Looking Ahead
In the next article in this series (#3 of 5), I’ll explore The ROI Proposition for Healthcare Communication Orchestration—why the financial, operational, and clinical returns are far greater than most health systems realize.
Orchestration isn’t just a technology play. It’s a pathway to safer, more efficient, more human-centered care.
- ECRI Top 10 Patient Safety Concerns (2025): https://home.ecri.org/blogs/ecri-thought-leadership-resources/top-10-patient-safety-concerns-2025
- https://pubmed.ncbi.nlm.nih.gov/40228297/
- Candello (CRICO) report (2025 – updated from 2015): https://www.candello.com/Insights/Candello-Reports/10-Year-Follow-Up-Comm?sc_camp=D0AFE79093214EF3844A5D1B9AFDE2BB#related-posts_e=0
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9745696/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11225068/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7786716/
- https://pubmed.ncbi.nlm.nih.gov/29317463/
- https://pubmed.ncbi.nlm.nih.gov/37339673/
Featured Resources
Related Articles