
Unified Communications: The Key to Solving Healthcare Inefficiencies
Hospitals are complex ecosystems where every second counts. From coordinating care teams to ensuring timely test results and patient handoffs, seamless communication is essential for delivering high-quality care. Yet, many hospitals still struggle with fragmented systems that create delays, errors, and frustration. While electronic medical records (EMRs) were designed to centralize patient data, they were not primarily designed to streamline real-time communication between clinicians. As a result, care teams waste valuable time searching for the right contact, waiting for responses, or navigating multiple systems—inefficiencies that slow down care, increase costs, and contribute to staff burnout. To keep patients moving efficiently through the healthcare system, hospitals need a unified communication platform that connects care teams in real time and ensures critical information reaches the right person at the right time.
Here’s the main problem: The EMR does not include everyone involved in coordinating the care of a patient, and it also does not know what everyone’s job is or when they are working. This makes it hard for the right information or message to get to the right person at the right time, creating widespread communication inefficiencies that erode both efficiency and patient outcomes.
These communication inefficiencies are the result of how healthcare team members interact with each other and with hospital systems in ways that erode value for patients, clinicians, and the hospital. They lead to poorer care, higher costs, and have a multimillion-dollar negative impact on every hospital in the US annually. In fact, 37% of hospitals are reporting losing money in 2025. Why is it so difficult to deliver effective patient care, maintain job satisfaction for staff, and run a profitable business? Administrators find it difficult to come up with a comprehensive solution because everyday inefficiencies appear as isolated incidents.
The challenge is that these breakdowns often appear as isolated issues—missing lab results, delayed callbacks, or misdirected messages—making them difficult to diagnose and resolve. But when viewed collectively, they reveal a broader pattern of operational waste tied to fragmented communication. Inefficiencies aren’t just frustrating—they’re expensive. According to the Peter G. Peterson Foundation, the healthcare system wastes up to $750 billion annually due to operational failures and poor care coordination. A significant portion of that waste comes from communication breakdowns—lost time searching for contacts, delays in getting test results, and incomplete information leading to poor decisions.
For clinical leaders and administrators, the constant stream of small glitches and miscommunications can feel overwhelming. But understanding these issues through the lens of communication inefficiencies provides a cohesive framework for identifying and solving the root problem. TigerConnect has identified seven key communication inefficiencies that frequently disrupt healthcare workflows:
- Searching for contacts: Clinicians often waste valuable time searching for the right contact due to outdated or inaccurate schedules, leading to frustration and delays.
- Mis-contacting: Contacting the wrong individual not only wastes time but also disrupts the workflow of both parties involved.
- Waiting for responses or results: A lack of steady information flow means care teams are left waiting for calls back or test results interrupting the continuity of care.
- Switching between multiple applications: Constantly toggling between different platforms and applications slows down workflows and reduces efficiency.
- Dealing with interruptions: Frequent alerts and pages, especially from outdated systems, significantly disrupt focus and increase cognitive load.
- Sifting through information: Clinicians face the challenge of navigating through disorganized information systems to find what they need, leading to inefficiency and frustration.
- Deciding with insufficient information: Receiving incomplete alerts, notifications, or messages that require clinicians to seek clarification before they can make a decision.
These problems don’t occur in isolation; rather, they are symptoms of a disjointed and fragmented system. It’s a critical time for hospitals to address these issues. Despite the benefits EMRs have brought to hospitals, they have not been successful at solving the massive communication issues that hospitals have today. That’s where a unified communication platform becomes essential. A properly designed and integrated CC&C platform can eliminate communication inefficiencies by connecting care teams across departments and beyond the hospital walls.
Care delivery is becoming more distributed—patients are receiving care not just in hospitals but also in outpatient facilities, urgent care centers, and even at home. This shift makes unified communication more critical than ever. Without it, communication gaps will only widen, amplifying existing inefficiencies. For hospitals to succeed financially and clinically, they need to focus on eliminating communication inefficiencies. A unified communication platform empowers care teams with real-time access to the right information and the right people, ensuring smoother workflows, better patient outcomes, and improved staff satisfaction.
Once you start looking for these inefficiencies, you’ll see opportunities for improvement everywhere. And with the right communication strategy, hospitals can not only improve efficiency but also improve care delivery and financial performance.
Featured Resources
Related Articles
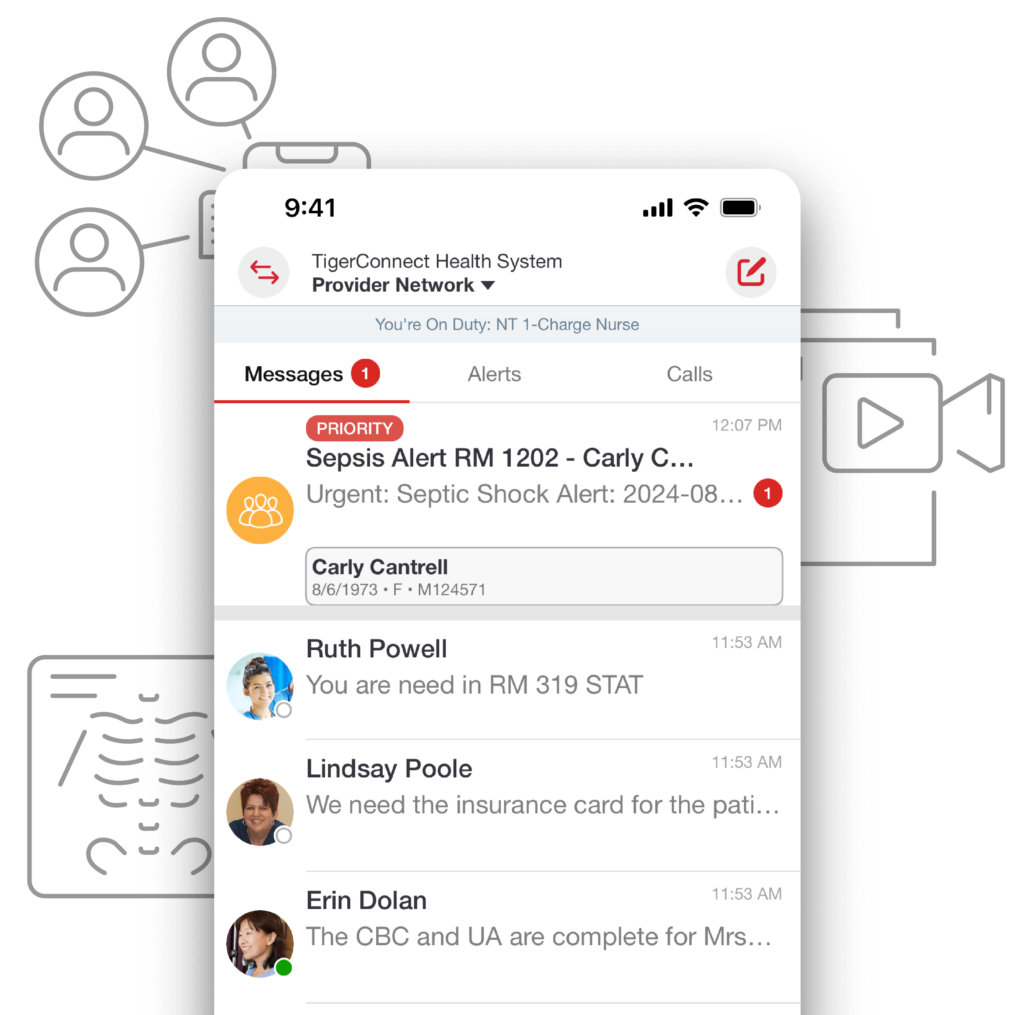
See TigerConnect Clinical Collaboration in Action
Book a demo to see how TigerConnect’s HIPAA-compliant, best-in-class collaboration platform can help clinicians and ancillary staff coordinate care more efficiently.






