Home / Blog /
How Data Standards in Healthcare Support Interoperability

How Data Standards in Healthcare Support Interoperability
I work on the EHR project team at an academic medical center. Over the past 23 years, I’ve helped design, build, and support data flows among unrelated homegrown and vendor database systems.
I appreciate data standards! They make my job much easier.
And what is my job? To support and improve patient care and patient safety by making data move more quickly, accurately, and securely.

Maybe the data is going from the lab system to the EHR to the doctor’s phone at the bedside, making crucial results available at the earliest possible moment. Or perhaps data is pushed from the credentialing database to the EHR to the ePrescribing vendor so the hospital’s newest physician can electronically prescribe medications. Or maybe a diabetes researcher needs endocrinology reports from the data warehouse.
Whatever the case, data standards make it easier for me to get the right data to the right person at the right time and place.
But there’s a lot of complexity behind those data transactions because each system has its own database, data definitions, and structures. Every day, for example, I push data from an Oracle database to a Caché database, and then pass that data to an Excel spreadsheet.
This isn’t a trivial feat. It’s like the children’s game “telephone.” The first child whispers a message to the second child, who whispers it to the third child, and so on. Unless each child receives the message correctly, stores it in their head correctly, and repeats it correctly (and they never do), the message is a mess when it gets to the end of the line.
Funny for kids, not so funny for patients. Patients need the full message to arrive quickly, accurately, and securely.
What Is Interoperability?
Interoperability refers to the ability of different IT systems with different infrastructures to share data accurately. Interoperability could not happen without data standards that establish rules for packaging the data.
It’s easy to understand when you consider something like electricity. What if U.S. electricians decided to start replacing our standard house outlets …

… with this version …

The standard is violated, and electricity cannot flow to your devices unless manufacturers create a compatible version of all their plugs.
Now, when it comes to healthcare, we have two types of interoperability.
-
- Interoperability within a single healthcare organization, like a hospital or clinic. Three examples are:
- Lab results flowing from the lab system to the EHR.
- Provider data flowing from the credentialing system to the scheduling system.
- Medication orders flowing from the EHR to the pharmacy system.
- Interoperability across disparate healthcare organizations or technologies. Three examples are:
- Patient data flowing from a fitness tracking device to a clinic’s EHR.
- Clinical data flowing from a hospital to a Health Information Exchange (HIE).
- Insurance validation data flowing from a hospital’s EHR to a patient’s insurance company and then back to the EHR.
Since the first type of interoperability exists within a single organization, we could call it intra-interoperability. And since the second type involves data flowing outside an organization, we could call it intra-interoperability.
We could. After all, who doesn’t want two more 10-syllable words?
I only point out the distinction to say the scope of this article is limited to the first type of interoperability: between disparate IT systems within one healthcare organization.
3 Benefits of Interoperability
Interoperability is challenging to implement because there are so many vendors with their own database systems and data structures.
There are also different data formats. Names, for example. Are they stored in mixed case or upper case? Do they support non-standard names like André and LaPage?
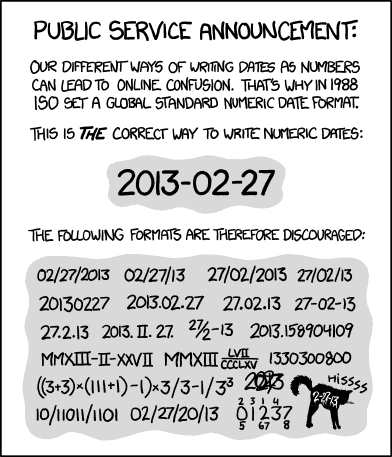
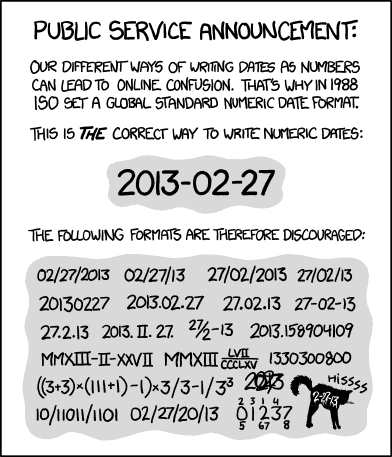
Or consider all the possibilities for dates.
But it’s worth solving these puzzles. Because here are three ways interoperability improves the healthcare system:
-
- Interoperability improves patient safety.
- Interoperability makes electronic Patient Health Information (ePHI) more secure.
- Interoperability promotes innovation.
Let’s look closer at each benefit.
Interoperability improves patient safety
Because computers work 24/7/365 and perform tasks repeatedly with zero errors, interoperability brings three wins for patient safety.
First, clinicians can have access to clinical data wherever they go. A nurse at her nursing station can add a note to the EHR, and the attending can view the note moments later on her mobile phone while sitting at Starbucks. The attending can get into her car and order a consult. The consulting physician can view an associated radiology image from his office back at the hospital. Through interoperability, clinicians make decisions based on up-to-date, accurate patient data everywhere they go, and patient safety is improved.
Second, interoperability speeds up the delivery of patient care. A critical lab result reaches the physician seconds after it is entered into the lab system, enabling the physician to immediately ePrescribe a vital medication that’s received seconds later in the pharmacy. Because of interoperability, clinical data flows swiftly to clinicians so they can make timely decisions and provide timely care, and patient safety is improved.
Third, since data flows faster and clinicians can access it wherever they go, reordering of tests, medications, and procedures happens infrequently. Clinicians either have access to the results, or they can confirm the order was placed. Because of interoperability, patients avoid unnecessary risks, and patient safety is improved.
Interoperability makes electronic Patient Health Information (ePHI) more secure
ePHI is more secure because interoperability confines data transfers to specified IT systems. Nobody needs to copy data to a file and transmit it across a network or (heaven forbid) email.
Also, many systems encrypt the data as it moves between systems, so if an evil entity happens to find it in transit, they won’t be able to use it.
Interoperability promotes innovation
If a vendor comes up with ingenious innovation, but their system cannot interact with other healthcare IT systems, its usefulness is limited.
Hank Hikspoors, Chief Technology Officer at T-System, says it best:
“Innovations without interoperability are essentially rendered useless because they have no real-world application and no influence on outcomes. Removing barriers to interoperability will not only drive future innovation but also ensure that those innovations can be successfully leveraged in order to make a difference in patient’s lives.”
How Data Standards in Healthcare Support Interoperability
How do we get to interoperability? Only by packaging and communicating data inconsistent, agreed-upon structures so receiving systems know what to do with it. This is what we mean by “data standards.” Without them, there are too many variables for computer programmers to consider. They’d rarely get it right.
This table summarizes some common data formatting and exchange standards seen in modern healthcare IT systems.
Standard
|
Description
|
| C-CDA |
Consolidated-Clinical Document Architecture: Structure for clinical documents containing both human-readable text and machine-readable XML |
| CSV |
Comma-Separated Values: Flexible structure for sending any number of fields for any number of records in one plain text file, separating each value with a comma |
| DICOM |
Digital Imaging and Communications in Medicine: Structure for medical imaging information |
| FHIR |
Fast Healthcare Interoperability Resources: Structures for specific data elements rather than entire health records or documents |
| HL7 |
Health Level Seven International: Multiple structures for various types of health information records, generated and sent by a computer one record at a time |
| JSON |
JavaScript Object Notation: Simple structure for sending any number of fields for a large but limited number of records in a text |
| QRDA |
Quality Reporting Document Architecture: Structure for healthcare quality measurement information |
| XML |
Extensible Markup Language: Flexible structure for sending any number of fields for any number of records in a text file |
Today, we have hundreds of vendors offering thousands of products and services intended to improve every piece of our healthcare system:
-
- Patient registration
- Patient scheduling
- Patient interactions
-
- Outpatient visits
- ER visits
- Hospital admissions
- Nurse call systems
- Order entry
- Lab tests
- Radiology images
- Medication orders and administration
- Referrals
- Telehealth
- Remote Patient Monitoring
- Surgeries
- Clinical Documentation
- Electronic Health Records (EHRs)
- Clinical communication and collaboration
- Health insurance
- Billing
- Healthcare analytics
- Reporting
- Research
- Provider credentialing
- Planning
- Marketing
How could so many unrelated systems hope to communicate with other systems? Sitting by themselves, each one has limited value.
Well, here’s the thing: Vendors can build their systems around any infrastructure they choose. If they include established data standards, their products and services can integrate with any other system that conforms to the same standards.
Plug and play. That’s interoperability, brought to you by Data Standards.
As a quick visual example, here’s a diagram of a system I used to manage. It pulled provider data from source systems, then sent that data throughout the enterprise, supporting the needs of seven mission-critical systems. You’ll notice a heavy dependency on the HL7 standard.
An Innovative Healthcare Application that Leverages Data Standards
Here’s a quick summary of where we are:
-
- Interoperability means IT systems can share data with each other.
- Interoperability brings at least three benefits to the healthcare system:
- Greater patient safety
- Greater ePHI security
- Greater innovation
- Interoperability is made possible by data standards that allow disparate IT systems to share data, even when different vendors created the systems around different infrastructures.
TigerConnect is one vendor helping us experience the full richness of interoperability through data standards in healthcare. They turn a clinician’s mobile phone or tablet into a potent weapon in the moment-by-moment fight against disease and suffering. At least that’s how I see it.
The power of TigerConnect lies in its real-time integrations:
-
- Major EHRs
- Lab results
- Radiology images
- Nurse call system
- Staffing and on-call schedules, including patient-specific care team membership
- Analytics
These integrations help organizations get the most value from their EHR by bringing the most essential clinical and staffing information right to the clinician’s phone, right at the point of care, wrapped in HIPAA-compliant text, voice, and video communications. It’s absolutely transformative.

Conclusions
This interoperability story is still emerging. FHIR is the newer, upcoming standard for data exchange. Vendors are just beginning to exploit it. The industry should see useful developments over the next five years.
In the meantime, I offer sincere thanks to all vendors who contribute to interoperability in healthcare, because I do NOT miss the days of copying a spreadsheet onto a 5¼” floppy disk and walking it to an office two buildings away from the hospital.
Tags: data standards in healthcare